Abstract
TGF-β1 and TGF-βR1 play important roles in immune and inflammatory responses. Genetic variants of TGF-β1 rs1800470 and TGF-βR1 rs334348 have emerged as potentially prognostic biomarkers for HPV-related head and neck cancer, while their prognostic effect on survival of smoking-related head and neck cancer remains unknown. This study included 1403 patients with smoking-related head and neck cancer, and all these patients were genotyped for TGF-β1 rs1800470 and TGF-βR1 rs334348. Both univariate and multivariate analyses were performed to evaluate associations between the two functional genetic variants in microRNA binding sites of TGF-β1 and TGF-βR1 and survivals. Patients with TGF-β1 rs1800470 CT or CC genotype had 30–35% risk reductions for OS, DSS, and DFS compared to patients with TT genotype among overall patients, ever smokers, and patients administered chemoradiation. Furthermore, patients with TGF-βR1 rs334348 GA or GG genotype had significant 50–60% risk reductions for OS, DSS, and DFS compared to patients with AA genotype among overall patients and patients administered chemoradiation; among ever smokers, the risk reductions even reached 60–70%. The TCGA dataset was used for validation. These findings suggest that TGF-β1 rs1800470 and TGF-βR1 rs334348 significantly affect survival outcomes in patients with smoking-related head and neck cancer, especially in the subgroups of ever smokers and patients treated with chemoradiation. These genetic variants may serve as prognostic indicators for patients with smoking-related head and neck cancer and could play a role in advancing the field of personalized chemoradiation, thereby improving patient survival and quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous cell carcinoma (HNSCC) is the seventh most common cancer globally and has a 5-year survival rate of 40–50%, and its incidence is increasing [1]. In 2020, there were nearly 1,000,000 new cases of HNSCC and over 400,000 fatalities from HNSCC around the world, highlighting the considerable threat to public health posed by this disease [1]. Although tobacco and alcohol are the most important etiologic agents in HNSCC, recently, it has been well recognized that approximately 10–20% of HNSCC, chiefly oropharyngeal cancer, are associated with high-risk HPV infection [2].
The smoking-related head and neck cancer is a key subtype of HNSCC that originates in the oral cavity, hypopharynx, and larynx and is predominantly associated with smoking and alcohol consumption, which is markedly aggressive and often accompanied by nonspecific symptoms during the early stages, so patients are susceptible to misdiagnosis and delayed diagnosis [3, 4]. Despite continuous enhancements in recent years in treatments for smoking-related head and neck cancer, including surgery, chemotherapy, and radiotherapy, the prognosis for patients with smoking-related head and neck cancer has not significantly improved [5]. Notably, patients diagnosed with smoking-related head and neck cancer who have similar clinical and pathological characteristics and receive the same therapeutic interventions sometimes experience substantially different clinical outcomes [6,7,8].
The vital role of smoking in the etiology of smoking-related head and neck cancer may be attributed in part to the detrimental effects of chemical compounds found in tobacco smoke, including reactive oxygen species and nitrogen species, on macromolecules such as lipids, proteins, and nucleic acids; furthermore, the oxidative stress generated by the interaction of smoking-induced oxygen species and nitrogen species plays a significant part in promoting inflammation and cancer progression [9]. Previous research elucidated that inflammatory cytokines may play a pivotal role in the prognosis of patients with smoking-related head and neck cancer [10]. However, research on utilizing biomarkers to predict the prognosis of patients with smoking-related head and neck cancer may be limited.
The host’s immune response and the reaction to chronic inflammation are significant biological contributors to both the oncogenesis and prognosis of smoking-related head and neck cancer [11]. Transforming growth factor β1 (TGF-β1) exerts a notable impact on tumor development and the immune microenvironment by modulating various cellular processes, including differentiation, proliferation, migration, and apoptosis [12]. Transforming growth factor β receptor 1 (TGF-βR1), a single-pass serine/threonine kinase receptor, is a vital downstream component within the TGF-β signaling cascade, and absence of TGF-βR1 affects the function of this pathway [13].
Several studies [14,15,16,17] have shown that single nucleotide polymorphisms (SNPs) within miRNA binding sites, such as TGF-β1 rs1800470 (merged from NCBI SNP rs1982073; T869C; codon 10 of exon 1; encoding Leu10Pro), which binds to miRNA-187, and TGF-βR1 rs334348, which binds to miRNA-628-5p, may predict the clinical outcomes of patients with breast cancer and oropharyngeal SCC via their potential function to exert influence on gene expression regulation. TGF-βR1 rs334348 is in strict linkage disequilibrium and is located in the 3’ untranslated region of TGF-βR1 [14]. These SNPs at miRNA binding sites may subsequently induce alterations in cellular homeostasis, ultimately contributing to an individual’s predisposition to cancer risk and impacting disease prognosis [14, 18, 19]. Findings also suggest the potential involvement of these single nucleotide polymorphisms in the predisposition to and progression of specific diseases, underscoring the prospective clinical relevance of these genetic variants [20, 21]. Notably, our most recent study suggested that both TGF-β1 rs1800470 and TGF-βR1 rs334348 might significantly affect the survival of patients with human papillomavirus (HPV)-associated oropharyngeal cancer [22], while it remains unknown whether the same genetic variants of TGF-β1 and TGF-βR1 impact the clinical outcomes of smoking-related head and neck cancer. Since these two functionally significant genetic variants of TGF-β1 and TGF-βR1 operate within the same pathway, it may allow us to evaluate the comprehensive impact of TGF-β1 rs1800470 and TGF-βR1 rs334348 on survival of smoking-related head and neck cancer [23]. Assessing effects of TGF-β1 rs1800470 and TGF-βR1 rs334348 might reveal stronger associations between individual TGF-β1 rs1800470 or TGF-βR1 rs334348 variants and outcomes for patients with smoking-related head and neck cancer.
In the present study, we assessed the association of TGF-β1 rs1800470 and TGF-βR1 rs334348 with the prognosis of patients with smoking-related head and neck cancer overall and stratified by smoking status and treatment. The discovery and analysis of genetic variants that carry significant prognostic value could help advance the development of tailored therapeutic strategies.
Materials and methods
Study patients
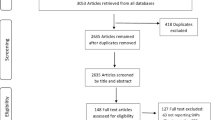
In a comprehensive molecular epidemiology investigation of HNSCC carried out at The University of Texas MD Anderson Cancer Center from January 1998 to September 2012, a total of 1403 consecutive patients diagnosed with smoking-related head and neck cancer, including SCC of oral cavity, SCC of hypopharynx, and SCC of larynx, were enrolled. The study targeted newly diagnosed individuals with histologically verified, previously untreated smoking-related head and neck cancer, imposing no limitations on factors such as age, sex, race and ethnicity, cancer stage, or histological classification. This study was approved by the Institutional Review Board of MD Anderson Cancer Center and was performed in accordance with the Declaration of Helsinki, and all participants provided written informed consent prior to enrollment. Upon entering the study, patients were asked to complete an epidemiological questionnaire encompassing demographic information and risk factors, including smoking and alcohol use status. Furthermore, a 30mL pretreatment blood sample was procured from each patient for genotyping. Throughout the treatment period and subsequent follow-up, patients underwent routine clinical assessments and radiological examinations [18]. In-depth information pertaining to patient enrollment, follow-up, and the epidemiological and clinical data collected from the study patients has been previously reported [24].
Genotyping of TGF-β1 rs1800470 and TGF-βR1 rs334348
Genomic DNA was extracted from leukocyte cell pellets with the QIAamp DNA Blood Mini Kit (QIAGEN Inc., Valencia, CA), following the manufacturer’s protocol. The genomic DNA was genotyped with the Illumina HumanOmniExpress-12v1 BeadChip as described in our previous paper [25]. For some patients with genotyping missing, genotyping was performed using the polymerase chain reaction–restriction fragment length polymorphism method as previously described [26]. Quality control measures were implemented, including repeated analysis of a randomly selected 10% of samples; results were 100% concordant with the initial results. For validation, the epidemiological, clinical, and survival data from the TCGA dataset and the genotyping of the 2 SNPs from the NIH dbGaP database were extracted on 312 smoking-related head and neck cancer patients, for whom such data was available for analysis.
Statistical analysis
The primary endpoints of this investigation were overall survival (OS), disease-specific survival (DSS), and disease-free survival (DFS). OS was defined as the time from the first appointment at The University of Texas MD Anderson Cancer Center to death from any cause or date of the last follow-up. Participants who were alive at the end of the study period or lost to follow-up were considered censored. DSS was defined as the time from the first appointment to death from disease or the date of the last follow-up. Recurrent disease was defined as the appearance of a new lesion of the same histology verified by biopsy (incisional, excisional, or needle biopsy), the reappearance of any lesion that had disappeared, or the development of tumor-related symptoms. DFS was computed from the date of the end of treatment to the date of the last follow-up or the date of clinically detectable recurrent cancer (local, regional, or distant). Participants who were recurrence free or lost to follow-up were considered censored.
SAS software (version 9.4; SAS Institute, Cary, NC) was used for all statistical analyses. All statistical tests were two-sided, with P < 0.05 deemed indicative of statistical significance. In the univariate analysis, we evaluated the survival impact of epidemiological and clinical factors, such as age, sex, race and ethnicity, smoking status, alcohol use status, index tumor stage, comorbid conditions, and treatment. Some variables that did not exhibit statistically significant prognostic value in the univariate analysis were nonetheless incorporated into the main-effects and final multivariable models, given their relevance in epidemiological and clinical contexts. We applied the Kaplan-Meier method to compare survival rates among smoking-related head and neck cancer patients with distinct genotypes and calculated the log-rank statistic to examine whether a significant difference in survival existed between the genotype groups. Furthermore, we assessed the statistical association between these genotypes and survival outcomes in smoking-related head and neck cancer patients. We used a Cox proportional hazards model to conduct this analysis, which integrated age, sex, race and ethnicity, smoking status, alcohol use status, disease stage, comorbid conditions, and treatment as covariates. We additionally conducted a multivariable analysis to assess the influence of functional genetic variants on survival by employing stratification according to smoking status and treatment. Finally, we conducted a multivariable analysis to examine the combined impact of TGF-β1 rs1800470 and TGF-βR1 rs334348 on survival, stratifying patients according to smoking status and treatment.
Results
Patient characteristics
Table 1 shows the demographic and clinical characteristics of the 1403 study patients. The median follow-up duration was 37.0 months (range 0.7 to 216.0). The mean age at diagnosis was 59.7 years (range 26 to 94). Of the 1403 patients, 960 (68.4%) were men, and 443 (31.6%) were women. A total of 1159 patients (82.6%) identified as non-Hispanic White, and 244 (17.4%), as another race and ethnicity. Among the patients, 1054 (75.1%) were ever smokers, and 1021 (72.8%) were ever alcohol drinkers. More than half of the patients (812; 57.9%) presented with stage III or IV disease. The primary treatment modality was chemoradiation for 908 patients (64.7%) and surgery for 495 (35.3%). A total of 615 patients died during follow-up, 259 from smoking-related head and neck cancer, and 359 patients had disease recurrence.
Association of TGF-β1 rs1800470 and TGF-βR1 rs334348 with survival
We observed that patients with CT or CC genotype of TGF-β1 rs1800470 experienced improved OS, DSS, and DFS compared to those with TT genotype (log-rank P = 0.001, P = 0.0043, P = 0.0079, respectively, Fig. 1). Furthermore, patients with CT or CC genotype had 30–35% reduced risks of death and recurrence compared to patients with TT genotype (adjusted hazard ratio [aHR], 0.70; 95% CI, 0.59 to 0.84 for OS; aHR, 0.66; 95% CI, 0.50 to 0.87 for DSS; and aHR, 0.71; 95% CI, 0.56 to 0.89 for DFS) (Table 2).
Patients with GA or GG genotype of TGF-βR1 rs334348 experienced improved OS, DSS, and DFS compared to those with AA genotype (all log-rank P < 0.0001, Fig. 2). In addition, patients with GA or GG genotype had 50–60% reduced risks of death and recurrence compared to patients with AA genotype (aHR, 0.42; 95% CI, 0.33 to 0.55 for OS; aHR, 0.42; 95% CI, 0.29 to 0.61 for DSS; and aHR, 0.49; 95% CI, 0.37 to 0.67 for DFS) (Table 2). When we combined variant genotypes of the 2 SNPs, we found that the patients with combined CT/CC and GA/GG genotypes and significantly much better survival outcomes (all log-rank, p < 0.0001; Fig. 3) and more reduced risk for the clinical outcomes compared with those with TT and AA genotypes of the 2 SNPs (aHR, 0.30 and 95% CI, 0.21-0.044 for OS; aHR, 0.22 and 95% CI, 0.12-0.043 for DSS; and aHR, 0.30 and 95% CI, 0.19–0.49 for DFS; respectively, Table 2).
Association of TGF-β1 rs1800470 and TGF-βR1 rs334348 with survival by smoking status
In the subset of ever smokers, patients with CT or CC genotype of TGF-β1 rs1800470 experienced improved OS, DSS, and DFS compared to those with TT genotype. Additionally, patients with GA or GG genotype of TGF-βR1 rs334348 experienced improved OS, DSS, and DFS compared to patients with AA genotype. Conversely, among never smokers, no significant differences by genotype were discerned in OS, DSS, or DFS (All log-rank: P = 0.354 for OS; P = 0.495 for DSS; and P = 0.809 for DFS for TGF-β1 rs1800470 and P = 0.171 for OS; P = 0.987 for DSS; and P = 0.790 for DFS for TGF-βR1 rs334348, respectively).
Among ever smokers, patients with CT or CC genotype of TGF-β1 rs1800470 had 30–35% reduced risks of death and recurrence, and patients with GA or GG genotype of TGF-βR1 rs334348 had 60–70% reduced risks of death and recurrence (aHR, 0.71; 95% CI, 0.58 to 0.87 for OS; aHR, 0.65; 95% CI, 0.48 to 0.88 for DSS; and aHR, 0.69; 95% CI, 0.53 to 0.89 for DFS for TGF-β1 rs1800470; aHR, 0.39; 95% CI, 0.30 to 0.52 for OS; aHR, 0.33; 95% CI, 0.21 to 0.53 for DSS; and aHR, 0.43; 95% CI, 0.30 to 0.62 for DFS for TGF-βR1 rs334348) (Table 3). In contrast, among never smokers, no significant associations were found between the genotypes of TGF-β1 rs1800470 and TGF-βR1 rs334348 and survival outcomes (Table 3).
Association of TGF-β1 rs1800470 and TGF-βR1 rs334348 with survival by treatment
Among the patients treated with chemoradiation, patients with CT or CC genotype of TGF-β1 rs1800470 experienced improved OS, DSS, and DFS compared to those with TT genotype, and patients with GA or GG genotype of TGF-βR1 rs334348 experienced improved OS, DSS, and DFS compared to those with AA genotype. Conversely, among patients treated with surgery only, no significant genotype-related differences were discerned in OS, DSS, or DFS (All log-rank: P = 0.110 for OS; P = 0.121 for DSS; and P = 0.325 for DFS for TGF-β1 rs1800470 and P = 0.171 for OS; P = 0.174 for DSS; and P = 0.270 for DFS for TGF-βR1 rs334348, respectively).
Among patients treated with chemoradiation, patients with CT or CC genotype of TGF-β1 rs1800470 had 30% reduced risks of death and recurrence, and patients with GA or GG genotype of TGF-βR1 rs334348 had 50–60% reduced risks of death and recurrence (aHR, 0.71; 95% CI, 0.57 to 0.87 for OS; aHR, 0.70; 95% CI, 0.52 to 0.94 for DSS; and aHR, 0.70; 95% CI, 0.54 to 0.92 for DFS for TGF-β1 rs1800470; aHR, 0.40; 95% CI, 0.30 to 0.54 for OS; aHR, 0.39; 95% CI, 0.26 to 0.60 for DSS; and aHR, 0.44; 95% CI, 0.30 to 0.63 for DFS for TGF-βR1 rs334348) (Table 4). In contrast, among patients treated with surgery only, no significant associations were found between the genotypes of TGF-β1 rs1800470 and TGF-βR1 rs334348 and survival outcomes (Table 4).
Validation for associations between TGF-β1 rs1800470 and TGF-βR1 rs334348 and survival outcomes using the TCGA dataset
For validation the findings mentioned above, a total of 312 smoking-related head and neck cancer patients with epidemiological, clinical, and survival data from the TCGA dataset as well as the genotyping data of the 2 SNPs from the NIH dbGaP were available for validation analysis (Table 5). As shown in Fig. 4, the similar survival differences from the TCGA patients were observed for the two SNPs, in particular, the differences of OS and DFS were statistically significant for TGF-βR1 rs334348 (Log-rank, p = 0.028 for OS and p = 0.049 for DFS, Fig. 4). Moreover, after adjustment with several prognostic confounders available in the TCGA dataset, the similar association patterns were observed among the patient in the TCGA for the 2 SNPs, especially the significant associations between the variant genotypes and risk of overall deaths and disease recurrence were found for TGF-βR1 rs334348 (aHR, 0.64 and 95% CI, 0.43–0.95 for OS and aHR, 0.63 and 95% CI, 0.40–0.98 for DFS, Table 6). The similar associations were found for TGF-βR1 rs334348 when the patients were stratified by patients’ smoking status (Table 7).
The OS, DSS, and DFS by TGF-β1 rs1800470 and TGF-βR1 rs334348 genotypes in the patients with smoking-related head and neck cancer from TCGA (N = 312). (A) OS estimated for TGF-β1 rs1800470 genotype, (B) DFS estimated for TGF-β1 rs1800470 genotype, (C) OS estimated for TGF-βR1 rs334348 genotype, and (D) DFS estimated for TGF-βR1 rs334348 genotype
Discussion
This study explored potential associations between the TGF-β1 rs1800470 and TGF-βR1 rs334348 genetic variants and the clinical outcomes of patients diagnosed with smoking-related head and neck cancer within a cohort of 1403 patients. Our findings suggest that these genetic variants are significantly associated with the risk of death and disease recurrence. Notably, the impact of the TGF-β1 rs1800470 and TGF-βR1 rs334348 genetic variants on clinical outcomes was particularly pronounced in the subgroups of ever smokers and patients treated with chemoradiation.
miRNAs, functioning as gene regulators, potentially contribute to cancer progression, increased susceptibility to cancer, and the prognosis of patients with cancer [27]. This involvement might be orchestrated through miRNA-mediated regulation of gene expression, which could be modulated by functional genetic variants residing within the miRNA binding sites; in particular, SNP within the miRNA binding sites of the 3’ untranslated region may play a role in the complex mechanisms underlying oncogenesis [17]. Previous studies demonstrated that TGF-β1 rs1800470 and TGF-βR1 rs334348 genetic variants located in the miRNA binding sites were critically associated with the risk of cancer development and clinical outcome for various cancers [14, 28]. Thus, comprehensive exploration of the associations between these genetic variants and clinical outcomes may pave the way for the establishment of more appropriate and precise personalized treatments.
Associations between the prognosis of smoking-related head and neck cancer and TGF-β1 rs1800470 and TGF-βR1 rs334348 were identified in several previous studies. Lundberg et al. [29] observed better OS and DFS in chemoradiotherapy-treated HNSCC patients carrying the C-allele of TGF-β1 rs1800470 than in patients carrying the TT genotype. Abakay et al. [30] focusing on primary laryngeal SCC within the Turkish population, found a noteworthy association between TGF-β1 polymorphisms and cancer susceptibility. In the patient cohort, a notable augmentation in the prevalence of the GC genotype and C allele associated with TGF-β1 rs1800471 was observed, indicating a significant association with susceptibility to laryngeal SCC. Conversely, no such association was evident for the TGF-β1 rs1800470. Our results suggest a protective role of the rs1800470 CT/CC in smoking-related head and neck cancer prognosis, the difference in these findings could be attributed to several factors including the ethnic composition of the study populations, the genetic background, the environmental exposures, and the specific characteristics of the patient cohorts, such as the tumor stage and treatment modalities. Moreover, these might be through mechanisms that involve a more effective immune response or a different pattern of cytokine expression. The functional genetic variants of TGF-β1 were verified via in vitro experiments. In a case-control study by Hu et al. [21]. , it was found that patients carrying the TGF-β1 rs1800469 -509T allele had a significantly reduced risk of developing nasopharyngeal carcinoma compared to those who did not carry this allele. Moreover, the mRNA expression level of -509CC and − 509CT was remarkably higher than that of -509TT in nasopharyngeal carcinoma tissues. Even though Hu et al. [21] found that the association between TGF-β1 rs1800470 and the survival of patients with nasopharyngeal carcinoma was not significant, they further elucidated that TGF-β1 functional genetic variants may affect malignancy susceptibility. Knobloch et al. [31] identified a significant association between TGF-βR1 rs334348 and both the occurrence and advancement of HNSCC. Chen et al. [32] discovered that the TGF-βR1 rs334348 polymorphism may modulate the progression of oral cancer by regulating the expression of TGF-βR1 and diminishing its ability to phosphorylate Smad-2 and Smad-3. Moreover, the researchers detected a synergistic association between TGF-βR1 rs334348 GA or GG genotype and the improved DSS of patients treated with radiotherapy, implying the potential clinical relevance of this genetic alteration in cancer management. In our present study, all patients with TGF-β1 rs1800470 CT or CC genotype and TGF-βR1 rs334348 GA or GG genotype had decreased risks of death and recurrence, and these associations were especially pronounced in the subgroups of ever smokers and patients treated with chemoradiation. These previous studies suggest a strong association between TGF-β1 and TGF-βR1 functional genetic variants and the prognosis of patients with smoking-related head and neck cancer, which supports our results and indicates the potential of TGF-β1 and TGF-βR1 to be a key factor in predicting patient’s treatment responsiveness and the prognosis of our studied patients.
Our previous findings [15, 18] demonstrated a notable association between TGF-β1 rs1800470 and survival in patients with HPV16-positive oropharyngeal cancer following definitive radiotherapy. These findings were consistent with our present study and imply that this genetic variant could induce a functional alteration and potentially influence treatment responses, impacting clinical results. However, the results of other studies across diverse cancer types may not be consistent with our current study’s findings concerning the impacts of TGF-β1 rs1800470 and TGF-βR1 rs334348. Both TGF-β1 rs1800470 and TGF-βR1 rs334348 act as oncogenes in gastric cancer. Juarez et al. [19] demonstrated that patients with gastric adenocarcinoma carrying the TGF-β1 rs1800470 TT or CT genotype had a decreased survival rate compared to those with the CC genotype. Similarly, He et al. [33] found a significant association between the TGF-βR1 rs334348 GG genotype and increased risk for gastric cancer. The differing prognostic relevance of TGF-β1 rs1800470 and TGF-βR1 rs334348 across an array of cancer types could be attributed to an assortment of factors, including the simultaneous existence of other oncogenic agents (e.g., HPV), the heterogeneity of tumors, differing molecular subclasses, and unique alterations within the tumor microenvironment.
Our present study suggests that TGF-β1 rs1800470 and TGF-βR1 rs334348 genetic variants may act as a protective factor in ever smokers with smoking-related head and neck cancer. The observed protective effect may be linked to the modulation of pro-inflammatory and immunosuppressive responses caused by smoking-induced expression and secretion of pro-inflammatory factors [10, 34, 35]. This process may alter responsiveness to treatment, thereby reducing the risk of mortality and disease recurrence. Intriguingly, when we stratified our cohort by smoking status and treatment, we found that the associations between TGF-β1 rs1800470 CT or CC and TGF-βR1 rs334348 GA or GG and prognosis were similar in ever smokers and patients treated with chemoradiation. This may be due to the DNA damage inflicted on cancer cells by radiotherapy and chemotherapy. Smoking-related head and neck cancer patients may also experience somatic genetic alterations, and these hypothetical functional genetic variants may enable a significant number of tumor cells to evade the immune system and apoptotic responses, thus resulting in variable sensitivity to chemoradiation. However, further studies are required to confirm these hypotheses.
The roles of TGF-β1 rs1800470 and TGF-βR1 rs334348 in cancer could potentially be explained by the fact that these polymorphisms are located in miRNA binding sites. Nicoloso et al. [14] explored the differences in function for TGF-β1 rs1800470 and TGF-βR1 rs334348 and found that the TGF-β1 rs1800470 polymorphism is situated at the miRNA187 binding site, with the T to C transition within this variant affecting the minimum free energy in the miRNA187::TGF-β1-mRNA complex. Moreover, Nicoloso et al. [14] performed the miR-187 luciferase assay and found that TGF-β1 rs1800470 affected protein levels of TGF-β1 by its genotypes, respectively. In addition, they evaluated the effect of TGF-βR1 rs334348 on miR-628-5p regulation of TGF-βR1. By overexpressing miR-628-5p in different cell lines, they observed the different effects of the genotypes of this single nucleotide polymorphism on the activity of TGF-βR1 protein levels in a cell-specific manner. This change in binding dynamics may influence miRNA gene regulation and the expression and functionality of TGF-β1 and TGF-βR1, potentially impacting both cancer susceptibility and prognosis.
The significantly greater effect of TGF-βR1 rs334348 than of TGF-β1 rs1800470 on reducing the risk of death and recurrence in patients with smoking-related head and neck cancer in the present study may be attributed to the location of TGF-β1 rs1800470 outside the 3’ untranslated region of TGF-β1, which might constrain its role in miRNA binding activity. We hypothesize that TGF-β1 rs1800470 could exert its influence through various mechanisms. From a biological standpoint, while the exact association of TGF-β1 rs1800470 with miRNA function remains an enigma, it is possible that TGF-β1 rs1800470 influences the expression level of TGF-β1 and the activity of the TGF-β1 signaling pathway. Such alterations could have downstream effects on biological processes, including cell proliferation, apoptosis, and inflammation [36]. The impact of these two single nucleotide polymorphisms on survival might function through an array of mechanisms, indicating the potential involvement of additional mediatory elements apart from the expression of the two respective genes [37]. The precise molecular mechanisms through which TGF-β1 rs1800470 and TGF-βR1 rs334348 impact the incidence and prognosis of smoking-related head and neck cancer require further exploration in both in vitro and in vivo experimental models.
To our knowledge, this is the first thorough research that further elucidates the associations between TGF-β1 rs1800470 and TGF-βR1 rs334348 and clinical outcomes in patients with smoking-related head and neck cancer overall and stratified by smoking status and treatment. These functional genetic variants markedly contribute to the reduction of death and disease recurrence risk among smoking-related head and neck cancer patients, particularly in ever smokers and patients treated with chemoradiation. Our findings suggest that utilizing pathway-based strategies may facilitate a more precise risk assessment in the future, leading to a deeper understanding of the etiology and prognosis of smoking-related head and neck cancer. Utilizing personalized treatment by considering each patient’s unique genetic makeup, enables a more targeted and effective intervention to combat the disease.
Our study has some limitations that should be addressed. First, as most of the patients were non-Hispanic White, the generalizability of our findings to other racial and ethnic populations may be limited, for which a larger study is needed for validation in other different genetic background. Second, the interpretation of some key findings in the stratified analysis may be constrained by the relatively small sample size within each subgroup. Third, given that the overarching study was both hospital-based and retrospective, potential selection and confounding biases may have impacted the patient cohort studied. Finally, considering the constraints of our limited sample size and fewer instances of outcome events in certain subsets, it is plausible that our findings deemed statistically significant may be attributable to random fluctuation. To bolster our conclusions, it would be beneficial to conduct additional studies that involve more participants.
Above all, our current research suggests that the TGF-β1 rs1800470 and TGF-βR1 rs334348 functional genetic variants may alter survival outcomes in smoking-related head and neck cancer patients, especially in the subgroups of ever smokers and patients treated with chemoradiation. These genetic variants may serve as prognostic predictors for patients with smoking-related head and neck cancer. They may play a role in advancing the field of personalized cancer therapy, thereby improving patient survival rates and quality of life. Nevertheless, for a thorough validation of these associations and the use of these variants as clinical prognostic biomarkers, additional research is needed to affirm our findings and further elucidate the molecular mechanisms underlying these observed associations.
Data availability
The data generated in this study are not publicly available due to information that could compromise patient privacy or consent but are available upon reasonable request from the corresponding author. The genotyping data from the genome-wide association study of SCC of head and neck from MD Anderson Cancer Center have been deposited in dbGaP (accession #: phs001173.v1.p1).
Abbreviations
- CI:
-
Confidence interval
- DFS:
-
Disease-free survival
- DSS:
-
Disease-specific survival
- HNSCC:
-
Head and neck squamous cell carcinoma
- HPV:
-
Human papillomavirus
- HR:
-
Hazard ratio
- miRNA:
-
microRNA
- OR:
-
odds ratio
- OS:
-
Overall survival
- SNP:
-
Single nucleotide polymorphism
- TGF-β1:
-
Transforming growth factor β1
- TGF-βR1:
-
Transforming growth factor β receptor 1
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Marks MA, Chaturvedi AK, Kelsey K et al (2014) Association of marijuana smoking with oropharyngeal and oral tongue cancers: pooled analysis from the INHANCE consortium. Cancer Epidemiol Biomarkers Prev 23:160–171. https://doi.org/10.1158/1055-9965.Epi-13-0181
Takes RP, Strojan P, Silver CE et al (2012) Current trends in initial management of hypopharyngeal cancer: the declining use of open surgery. Head Neck 34:270–281. https://doi.org/10.1002/hed.21613
Khariwala SS, Hatsukami DK, Stepanov I, Rubin N, Nelson HH (2018) Patterns of Tobacco Cessation attempts and symptoms experienced among smokers with Head and Neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg 144:477–482. https://doi.org/10.1001/jamaoto.2018.0249
Mody MD, Rocco JW, Yom SS, Haddad RI, Saba NF (2021) Head and neck cancer. Lancet 398:2289–2299. https://doi.org/10.1016/s0140-6736(21)01550-6
Moon PK, Ma Y, Megwalu UC (2022) Head and Neck Cancer Stage at Presentation and Survival outcomes among native hawaiian and other Pacific Islander patients compared with Asian and White patients. JAMA Otolaryngol Head Neck Surg 148:636–645. https://doi.org/10.1001/jamaoto.2022.1086
Caudell JJ, Torres-Roca JF, Gillies RJ, Enderling H, Kim S, Rishi A, Moros EG, Harrison LB (2017) The future of personalised radiotherapy for head and neck cancer. Lancet Oncol 18:e266–e73. https://doi.org/10.1016/s1470-2045(17)30252-8
Dubey P, Gupta R, Mishra A, Kumar V, Bhadauria S, Bhatt MLB (2022) Evaluation of correlation between CD44, radiotherapy response, and survival rate in patients with advanced stage of head and neck squamous cell carcinoma (HNSCC). Cancer Med 11:1937–1947. https://doi.org/10.1002/cam4.4497
Caliri AW, Tommasi S, Besaratinia A (2021) Relationships among smoking, oxidative stress, inflammation, macromolecular damage, and cancer. Mutat Res Rev Mutat Res 787:108365. https://doi.org/10.1016/j.mrrev.2021.108365
Zhang C, Sturgis EM, Zheng H, Zafereo ME, Wei Q, Li G (2014) TNF-α promoter polymorphisms and risk of recurrence in patients with squamous cell carcinomas of the nonoropharynx. Int J Cancer 135:1615–1624. https://doi.org/10.1002/ijc.28793
Valdes M, Villeda J, Mithoowani H, Pitre T, Chasen M (2020) Inflammatory markers as prognostic factors of recurrence in advanced-stage squamous cell carcinoma of the head and neck. Curr Oncol 27:135–141. https://doi.org/10.3747/co.27.5731
Heldin CH, Moustakas A (2016) Signaling receptors for TGF-β family members. Cold Spring Harb Perspect Biol. 810.1101/cshperspect.a022053
Liu J, Johnson K, Li J et al (2011) Regenerative phenotype in mice with a point mutation in transforming growth factor beta type I receptor (TGFBR1). Proc Natl Acad Sci U S A 108:14560–14565. https://doi.org/10.1073/pnas.1111056108
Nicoloso MS, Sun H, Spizzo R et al (2010) Single-nucleotide polymorphisms inside microRNA target sites influence tumor susceptibility. Cancer Res 70:2789–2798. https://doi.org/10.1158/0008-5472.Can-09-3541
Tao Y, Sturgis EM, Huang Z, Sun Y, Dahlstrom KR, Wei Q, Li G (2018) A TGF-β1 genetic variant at the miRNA187 binding site significantly modifies risk of HPV16-associated oropharyngeal cancer. Int J Cancer 143:1327–1334. https://doi.org/10.1002/ijc.31530
Martelossi Cebinelli GC, Paiva Trugilo K, Badaró Garcia S, Brajão de Oliveira K (2016) TGF-β1 functional polymorphisms: a review. Eur Cytokine Netw 27:81–89. https://doi.org/10.1684/ecn.2016.0382
Pelletier C, Weidhaas JB (2010) MicroRNA binding site polymorphisms as biomarkers of cancer risk. Expert Rev Mol Diagn 10:817–829. https://doi.org/10.1586/erm.10.59
Tao Y, Sturgis EM, Huang Z, Wang Y, Wei P, Wang JR, Wei Q, Li G (2018) TGFβ1 genetic variants predict clinical outcomes of HPV-Positive Oropharyngeal Cancer patients after definitive Radiotherapy. Clin Cancer Res 24:2225–2233. https://doi.org/10.1158/1078-0432.Ccr-17-1904
Juarez I, Gutierrez A, Vaquero-Yuste C, Molanes-López EM, López A, Lasa I, Gómez R, Martin-Villa JM (2021) TGFB1 polymorphisms and TGF-β1 plasma levels identify gastric adenocarcinoma patients with lower survival rate and disseminated disease. J Cell Mol Med 25:774–783. https://doi.org/10.1111/jcmm.16131
Sultana TN, Chaity NI, Hasan MM et al (2023) TGFβ1 rs1800469 and SMAD4 rs10502913 polymorphisms and genetic susceptibility to colorectal cancer in Bangladeshi population. Mol Biol Rep 50:1393–1401. https://doi.org/10.1007/s11033-022-08146-x
Hu S, Zhou G, Zhang L, Jiang H, Xiao M (2012) The effects of functional polymorphisms in the TGFβ1 gene on nasopharyngeal carcinoma susceptibility. Otolaryngol Head Neck Surg 146:579–584. https://doi.org/10.1177/0194599811434890
Niu Z, Sun P, Liu H et al (2023) Functional genetic variants in TGF-β1 and TGF-βR1 in microRNA binding sites predict outcomes in patients with HPV-positive oropharyngeal squamous cell carcinoma. Clin Cancer Res Doi. https://doi.org/10.1158/1078-0432.Ccr-23-1161
Wang J, Xiang H, Lu Y, Wu T (2021) Role and clinical significance of TGF–β1 and TGF–βR1 in malignant tumors (review). Int J Mol Med 47. https://doi.org/10.3892/ijmm.2021.4888
Guan X, Sturgis EM, Lei D, Liu Z, Dahlstrom KR, Wei Q, Li G (2010) Association of TGF-beta1 genetic variants with HPV16-positive oropharyngeal cancer. Clin Cancer Res 16:1416–1422. https://doi.org/10.1158/1078-0432.Ccr-09-2877
Shete S, Liu H, Wang J et al (2020) A Genome-Wide Association Study Identifies Two Novel Susceptible Regions for Squamous Cell Carcinoma of the Head and Neck. Cancer Res 80:2451–2460. https://doi.org/10.1158/0008-5472.Can-19-2360
Yuan X, Liao Z, Liu Z et al (2009) Single nucleotide polymorphism at rs1982073:T869C of the TGFbeta 1 gene is associated with the risk of radiation pneumonitis in patients with non-small-cell lung cancer treated with definitive radiotherapy. J Clin Oncol 27:3370–3378. https://doi.org/10.1200/jco.2008.20.6763
Garcia Mesa K, Bermejo JL, Torres D, Gilbert M, Plass C, Hamann U (2020) Genetic variability in the microRNA binding sites of BMPR1B, TGFBR1, IQGAP1, KRAS, SETD8 and RYR3 and risk of breast Cancer in Colombian women. Onco Targets Ther 13:12281–12287. https://doi.org/10.2147/ott.S274431
Syed V (2016) TGF-β signaling in Cancer. J Cell Biochem 117:1279–1287. https://doi.org/10.1002/jcb.25496
Lundberg M, Saarilahti K, Mäkitie AA, Mattila PS (2010) TGFbeta1 genetic polymorphism is associated with survival in head and neck squamous cell carcinoma independent of the severity of chemoradiotherapy induced mucositis. Oral Oncol 46:369–372. https://doi.org/10.1016/j.oraloncology.2010.02.012
Abakay CD, Pashazadeh M, Ardahanli E, Oral HB (2020) Transforming growth factor-β1 gene polymorphism as a potential risk factor in Turkish patients with laryngeal squamous cell carcinoma. J Cancer Res Ther 16:144–149. https://doi.org/10.4103/jcrt.JCRT_598_19
Knobloch TJ, Lynch MA, Song H et al (2001) Analysis of TGF-beta type I receptor for mutations and polymorphisms in head and neck cancers. Mutat Res 479:131–139. https://doi.org/10.1016/s0027-5107(01)00157-9
Chen L, Chen F, Wang X et al (2020) Prognostic value of transforming growth factor beta receptor 1 polymorphisms in patients with oral cancer. J Oral Pathol Med 49:137–144. https://doi.org/10.1111/jop.12967
He B, Xu T, Pan B et al (2018) Polymorphisms of TGFBR1, TLR4 are associated with prognosis of gastric cancer in a Chinese population. Cancer Cell Int 18:191. https://doi.org/10.1186/s12935-018-0682-0
Mebratu YA, Smith KR, Agga GE, Tesfaigzi Y (2016) Inflammation and emphysema in cigarette smoke-exposed mice when instilled with poly (I:C) or infected with influenza A or respiratory syncytial viruses. Respir Res 17:75. https://doi.org/10.1186/s12931-016-0392-x
Malm IJ, Rooper LM, Bishop JA, Ozgursoy SK, Hillel AT, Akst LM, Best SR (2019) Molecular and immunologic analysis of laryngeal squamous cell carcinoma in smokers and non-smokers. Am J Otolaryngol 40:213–217. https://doi.org/10.1016/j.amjoto.2018.11.009
Colak S, Ten Dijke P (2017) Targeting TGF-β signaling in Cancer. Trends Cancer 3:56–71. https://doi.org/10.1016/j.trecan.2016.11.008
MacKinnon DP, Fairchild AJ, Fritz MS (2007) Mediation analysis. Annu Rev Psychol 58:593–614. https://doi.org/10.1146/annurev.psych.58.110405.085542
Acknowledgements
The authors gratefully thank Stephanie Deming from Editing Services, Research Medical Library, MD Anderson Cancer Center, for editing the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception and design: ZN, PS, NDG, MEZ, GL. Development of methodology: ZN, PS, GL. Acquisition of data: NDG, MEZ, GAC, GL. Analysis and interpretation of data: ZN, PS, PW, HL, JW, SJ, QW, GAC, GL. Writing, review, and/or revision of the manuscript: All authors. The work reported in the paper has been performed by the authors, unless clearly specified in the text.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board of MD Anderson Cancer Center, USA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Niu, Z., Sun, P., Zafereo, M.E. et al. TGF-β1 and TGF-βR1 variants are associated with clinical outcomes in smoking-related head and neck cancer patients treated with chemoradiation through modulating microRNA-mediated regulation. Cancer Immunol Immunother 73, 85 (2024). https://doi.org/10.1007/s00262-024-03672-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00262-024-03672-y