Abstract
Transfusion reactions induced by platelet transfusions may be reduced and alleviated by leukocyte reduction of platelets. Although leukoreduction of apheresis platelets can be performed either pre-storage or post-storage, seldom studies directly compare the incidence of transfusion reaction in these two different blood products. We conducted a retrospective study to compare the transfusion reactions between pre-storage and post-storage leukoreduced apheresis platelets. We reviewed the general characteristics and the transfusion reactions, symptoms, and categories for inpatients who received pre-storage or post-storage leukoreduced apheresis platelets. Propensity-score matching was performed to adjust for baseline differences between groups. A total of 40,837 leukoreduction apheresis platelet orders were reviewed. 116 (0.53%) transfusion reactions were reported in 21,884 transfusions with pre-storage leukoreduction, and 174 (0.91%) reactions were reported in 18,953 transfusions with post-storage leukoreduction. Before propensity-score matching, the odds ratio for transfusion reactions in the pre-storage group relative to the post-storage group was 0.57 (95% confidence interval [CI] 0.45–0.72, P < 0.01); the odds ratio after matching was 0.63 (95% CI 0.49–0.80, P < 0.01). A two-proportion z-test revealed pre-storage leukoreduction significantly decreases the symptoms of chills, fever, itching, urticaria, dyspnea, and hypertension as compared with those in post-storage leukoreduction. Pre-storage leukoreduced apheresis platelet significantly decreased febrile non-hemolytic transfusion reaction as compared with post-storage groups. This study suggests pre-storage leukoreduction apheresis platelet significantly decreases the transfusion reaction as compared with those in post-storage leukoreduction.
Similar content being viewed by others
Introduction
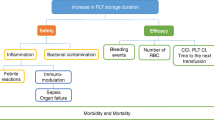
Transfusion reactions are a major issue in transfusion medicine. Platelet transfusion can be accompanied by adverse reactions, and transfusion reactions are more frequent after the transfusion of platelets than after transfusion of other blood products [1, 2]. Platelet products can be divided into pooled donor platelet concentrates and single-donor apheresis platelets. Apheresis platelets have been widely applied in clinical practice because they provide several advantages over pooled donor concentrates, such as reduced exposure to donor antigens and lower risk of septic transfusion reactions [3]. Leukoreduction is another important strategy for preventing transfusion reactions. Removal of leukocytes from platelet products may reduce the risk of human leukocyte antigen (HLA) alloimmunization and platelet refractoriness [4, 5], reduce the severity and frequency of febrile non-hemolytic transfusion reactions (FNHTRs) [6,7,8], and lower the risk of cytomegalovirus transmission [9, 10]. For apheresis platelets, the leukoreduction process can be performed either before or after the platelets stored. Pre-storage leukoreduction removes leukocytes during the preparation of apheresis platelets, whereas post-storage leukoreduction removes leukocytes by filter from unmanipulated apheresis platelets during the transfusion process at bedside. Pre-storage leukoreduction is generally believed to be superior to post-storage leukoreduction in preventing transfusion reactions because the former method reduces cytokine release from leukocytes while the platelet product is in storage [11]. However, seldom studies have compared these two modalities of transfusion reaction prevention, especially for apheresis platelets. In Taiwan, the Taiwan Blood Service Foundation has been promoting pre-storage leukoreduction apheresis platelets since 2012. However, they continue to simultaneously provide both pre-storage leukoreduction apheresis platelets and non-leukoreduction apheresis platelets. Therefore, we conducted a retrospective study to compare the transfusion reactions between pre-storage and post-storage leukoreduced apheresis platelets by using a propensity-score-matching analysis.
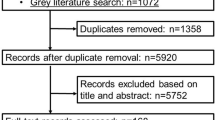
Methods
Transfusion order review and enrollment criteria
We retrospectively reviewed all leukoreduced apheresis platelet transfusion orders for inpatients in Taipei Veterans General Hospital from August 2018 to December 2022. Data on each patient’s age, sex, blood type, and admission ward were obtained for analysis. Pooled platelet concentrate transfusions were excluded from this study. Additionally, transfusions for outpatients, pediatric patients less than 1-year-old, and patients admitted to the emergency department or intensive care unit were excluded. This study was approved by the Institutional Ethical Committee of Taipei Veterans General Hospital, and the study protocol was in agreement with the Helsinki Declaration of 1975, revised in 2008.
Leukoreduction manufacturing process for apheresis platelets
Pre-storage leukoreduced apheresis platelets were prepared by the Taiwan Blood Service Foundation under the standard procedures. Platelets were collected using a leukocytapheresis device—Trima Accel®(Terumo BCT, USA), achieving a three-log reduction of leukocytes during apheresis [12, 13]. Post-storage leukoreduction was accomplished using a high-efficiency leukocyte filter—Haemonetics PXL8Y®(Haemonetics, USA) during the transfusion process at bedside [14]. Both pre-storage and post-storage leukoreduced apheresis platelets contained less than 5 × 106 leukocytes per unit, as per the standards of the Association for the Advancement of Blood and Biotherapies [15].
Transfusion reaction record and review
Patient vital signs, such as body temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation, were checked before transfusion. Vital signs were monitored every 15 min until the transfusion was complete. Patients were subsequently monitored for 60 min after the platelet transfusion was completed. During and after transfusion, any onset of new symptoms that indicated a potential transfusion reaction, such as chills, fever, itching, face flushing, urticarial, nausea, dyspnea, stridor, hypotension, cold sweating, hypertension, and chest pain, were recorded. These patients were referred to transfusion medicine physicians for further investigation. Every transfusion reaction was independently reviewed by two transfusion medicine physicians. Each documented transfusion reaction, including the reaction categories and symptoms, were recorded in the patient’s chart.
Statistical analysis
Each patient’s age, sex, blood type, admission ward, transfusion reaction, reaction category, and transfusion reaction-related symptoms are presented as number (n) and proportion (%). Logistic regression was used to determine the association between transfusion reactions and both pre-storage and post-storage leukoreduced apheresis platelets. A multivariate analysis adjusted for sex, age, and other clinical variables was performed to investigate the association between transfusion reactions and leukocyte-reduced apheresis platelets.
Propensity-score matching was performed to adjust for baseline differences between the pre-storage and post-storage groups [16]. Propensity score matching entails the selection of subsets from pre-storage leukoreduction group and post-storage leukoreduction group with similar covariate distributions, represented by propensity scores. This process aims to control for the confounding effects of covariates that might introduce bias into the estimated treatment effects. In 1-to-1 matching based on propensity scores, pre-storage subject are matched to post-storage subject, aligning the sample sizes between paired groups and ensuring similarity. Given the nature of this retrospective study, there were some inherent baseline differences (standardized mean difference > 0.1) in the original unmatched population between recipients of pre-storage and post-storage leukoreduced apheresis platelet transfusions. Propensity scores were generated through logistic regression by using pre-storage leukoreduction apheresis platelets as the dependent variable. Independent variables included age, sex, blood type, and admission ward. Propensity scores were obtained and applied to adjust for covariates in matched cases among pre-storage and post-storage leukoreduced apheresis platelet transfusions. Covariates were balanced between the matched groups and subsequently verified by the standardized mean difference. The conditional logistic regression was applied to determine the association between pre-storage leukoreduced apheresis platelets and transfusion reaction outcomes in paired groups after propensity-score matching. Logistic regression results are presented as odds ratio and 95% confidence interval (CI). Transfusion reaction categories and transfusion-related symptoms were compared using two proportion z-tests for pre-storage and post-storage leukoreduced apheresis platelets. Statistical tests were two-sided, and results were considered significant at P < 0.05. All analyses were performed using the R statistical software (The R Project for Statistical Computing, version 4.0.2).
Results
Characteristics and transfusion reactions of patients who received pre-storage or post-storage leukoreduced apheresis platelets
A total of 40,837 leukoreduced apheresis platelet transfusion orders were reviewed; 21,884 orders involved pre-storage leukoreduction and 18,953 orders involved post-storage leukoreduction. Detailed information relevant to the general characteristics of patients receiving pre-storage and post-storage leukoreduced apheresis platelets is shown in Table 1. The median age of the patients who received transfusions was 63 years (interquartile range: 51–73), and 55.8% were men. The majority of patients has blood type O, which is the most common blood type in Taiwan. Additionally, more than half of the transfusions were administered to cancer patients. Because this was a retrospective study, there were some inherent baseline differences (standardized mean difference > 0.1) between recipients of pre-storage and post-storage leukoreduced apheresis platelet transfusions: admission to neurology ward and age at 60 ~ 80 years old would receive more pre-storage leukoreduced apheresis platelet transfusion. We performed propensity-score matching to adjust for covariates between the pre-storage and post-storage cohorts and verified that by the standardized mean difference for each covariate less than 0.1. By propensity-score matching, a total of 18,314 matched cases were selected from original 18,953 post-storage and 21, 884 pre-storage. The histogram demonstrating propensity scores before and after matching is illustrated in Supplemental Fig. 1.
Transfusion reaction–related symptoms in patients who received pre-storage or post-storage leukoreduced apheresis platelets
Detailed information about transfusion reaction–related symptoms is shown in Table 2. A total of 211 and 347 transfusion reaction-related symptoms were reported in the pre-storage and post-storage leukoreduction groups, respectively. Itching was the most common symptom in pre-storage leukoreduction groups, while urticaria was the most frequent reported in post-storage. By two-proportion z-test analysis, the unmatched cohort showed that the pre-storage leukoreduction significantly decreased the symptoms of chills, fever, itching, urticaria, dyspnea, and hypertension as compared with those in post-storage leukoreduction. Other transfusion reaction symptoms, such as face flushing, nausea, vomiting, stridor, hypotension, syncope, cold sweating, pharyngeal edema, shock, and chest pain were not significantly different between pre-storage and post-storage leukoreduction groups. In propensity-score matched cohort, the pre-storage leukoreduction groups remained significantly lower symptoms of fever, chill, urticaria, dyspnea, and hypertension, but not itching. Figure 1 shows the incidence of transfusion reaction–related symptoms as well as comparison between pre-storage and post-storage leukoreduction apheresis platelet transfusion in unmatched and propensity-score matched cohort.
Transfusion reaction comparison between pre-storage and post-storage leukoreduced apheresis platelets
Statistical results are shown in Table 3. A total of 116 transfusion reactions were reported among 21,884 pre-storage leukoreduced apheresis platelet transfusions, and 174 reactions were reported among 18,953 post-storage leukoreduced transfusions. The statistical analyses revealed the pre-storage leukoreduced apheresis platelet significantly decrease the transfusion reaction as compared the post-storage groups in all statistical analysis, including crude rate, multivariate analysis adjusted for sex, age, and other covariates, as well as conditional logistic regression after propensity-score matching.
Transfusion reaction category comparison in pre-storage and post-storage leukoreduced apheresis platelets
The transfusion reaction categories are shown in Table 4. The two proportion z-test analysis revealed the pre-storage leukoreduced apheresis platelet significantly decreased FNHTR as compared with post-storage groups. These results remained significant in propensity-score matched cohort.
Discussion
Removal of leukocytes from blood products has been shown to reduce HLA alloimmunization, FNHTR, and platelet refractoriness. A randomized controlled clinical trial assigned eligible patients to receive either un-manipulated or leukoreduced blood products [17]. This study revealed no significant difference in in-hospital mortality, hospital length of stay, and total hospital cost between un-manipulated and leukoreduced blood products; however, patients who received leukoreduced blood products had a lower incidence of febrile reactions [17]. Most of the studies mentioned above involved pooled platelet concentrates. However, single-donor apheresis platelet transfusion has several advantages over pooled platelet concentrate transfusions, such as lower donor HLA exposure, less inventory and pooling, easier HLA matching, and reduced risk of septic transfusion reactions. Therefore, apheresis platelets have become the preferred platelet product, but few studies have focused on the effects of pre-storage versus post-storage leukoreduction in platelet apheresis. A recent study observed that FNHTR incidence was 0.07% in leukoreduced single donor apheresis platelets, 0.16% in pre-storage leukoreduced pooled platelets, 0.30% in post-storage leukoreduced pooled platelets, and 0.20% in non-leukoreduced pooled platelets [8]. These results imply that single-donor apheresis platelets may be superior to pooled platelets, regardless of the application or timing of leukoreduction in the pooled platelet products. However, it is not clear if pre-storage leukoreduction is superior to post-storage leukoreduction in apheresis platelet products. Furthermore, Mishima et al. [18] found that compared with bedside leukoreduction, universal leukoreduction was associated with a significantly higher rate of antibody detection (8.7% vs. 5.4%) and platelet transfusion refractoriness (7.3% vs. 3.2%). Therefore, it is worth investigating whether pre-storage leukoreduction platelet apheresis prevent more transfusion reaction. Our study exactly provides the evidence of pre-storage leukoreduced platelet apheresis significantly deceasing the transfusion reaction as compared with post-storage in a relatively large cohort research.
FNHTR is a very common transfusion reaction, and substantial research has revealed several underlying mechanisms of this reaction. Donor-derived leukocytes may interact with the recipient’s anti-leukocyte antibodies as a result of the antigen–antibody complement reaction and cytokine release [6]. This interaction can be mitigated by leukocyte removal through either pre-storage or post-storage leukoreduction. Leukocytes also release pyrogenic cytokines, such as interleukin-6, interleukin-8, tumor necrosis factor-alpha, and interleukin-1, which are believed to contribute to transfusion reactions. One advantage of pre-storage leukoreduction over post-storage leukoreduction is the minimization of cytokine accumulation during storage. This is a general reason why pre-storage leukoreduction is superior to post-storage leukoreduction [19]. In addition to cytokines released from leukocytes, the secretion of alpha granules and granular platelet chemokines can also induce transfusion reactions. The platelet-derived chemokines CCL3, CCL5, and CXCL4 can cause FNTHR [20, 21]. Neither pre-storage nor post-storage leukoreduction can filter out these platelet-derived chemokines and granules. This may explain although pre-storage leukoreduction platelet apheresis could alleviate the transfusion reaction more efficiently, it could not eliminate all the transfusion reaction.
In addition to decrease transfusion reaction, there are several well-known advantages and disadvantages of pre-storage leukoreduction. For example, a study found that pre-storage leukoreduction reduced not only the release of inflammatory cytokines from leukocytes but also the risk of virus transmission due to the release of intracellular organisms from leukocytes during storage [15]. Additionally, it is easier to control the quality of leukocyte removal in a donor center rather than at bedside. The major disadvantages of pre-storage or universal leukoreduction are the cost involved and the inherent issue of inventory management, as it is difficult to estimate the demand for leukoreduced platelets at the time of blood product preparation [22]. However, post-storage or bedside leukoreduction could be selectively applied to certain populations for which leukoreduced blood products are recommended, which could mitigate cost issues. In our study, the crude rate of transfusion reactions for pre-storage and post-storage leukoreduction groups was 0.53% and 0.91%, respectively. The number needed to treat to avoid one transfusion reaction with pre-storage rather than post-storage leukoreduced platelets was 263. This implies that for every 263 transfusions, one transfusion reaction could be prevented by opting for pre-storage leukoreduction platelet transfusion over post-storage leukoreduction. A cost-effective analysis should be considered when implementing pre-storage or post-storage apheresis platelet transfusions.
Our study had several inherent limitations. First, this was a retrospective study rather than a randomized controlled trial, so the baseline characteristics of the patients differed between the pre-storage and post-storage groups. Therefore, we performed propensity-score matching for the cohort to minimize potential selection bias. Second, only inpatients were included in the cohort to facilitate the follow-up and monitoring of transfusion reactions. Although our results may be generalizable to the majority of inpatients, this cohort is not representative of the entire transfusion candidate population. Third, our study focused on acute transfusion reactions but did not compare alloimmunization or platelet refractoriness between the pre-storage and post-storage groups. Finally, blood product selection should be dependent on each patient’s characteristics. A large-scale, randomized controlled clinical trial is necessary to identify the characteristics of patients who may benefit from pre-storage leukoreduced apheresis platelet transfusions.
Conclusion
In conclusion, this study suggests pre-storage leukoreduction apheresis platelet significantly decreases the transfusion reaction as compared with those in post-storage leukoreduction, especially in FNHTR. The crude rate of transfusion reactions for pre-storage and post-storage leukoreduction groups was 0.53% and 0.91%, respectively. The number needed to treat to avoid one transfusion reaction with pre-storage rather than post-storage leukoreduced platelets was 263. This study suggests that pre-storage leukoreduction apheresis platelet is an optimal choice in the supply of blood products.
Funding
This study is partially supported by the grants from Taipei Veterans General Hospital-National Yang-Ming University Excellent Physician Scientist Cultivation Program, No.112-V-A-072, Szu-Yuan Research Foundation of Internal Medicine.
References
Kiefel V (2008) Reactions induced by platelet transfusions. Transfus Med Hemother 35(5):354–358. https://doi.org/10.1159/000151350
Oakley FD, Woods M, Arnold S, Young PP (2015) Transfusion reactions in pediatric compared with adult patients: a look at rate, reaction type, and associated products. Transfusion 55(3):563–570. https://doi.org/10.1111/trf.12827
Ness PM, Campbell-Lee SA (2001) Single donor versus pooled random donor platelet concentrates. Curr Opin Hematol 8(6):392–396. https://doi.org/10.1097/00062752-200111000-00013
Slichter SJ, Davis K, Enright H, Braine H, Gernsheimer T, Kao KJ, Kickler T, Lee E, McFarland J, McCullough J, Rodey G, Schiffer CA, Woodson R (2005) Factors affecting posttransfusion platelet increments, platelet refractoriness, and platelet transfusion intervals in thrombocytopenic patients. Blood 105(10):4106–4114. https://doi.org/10.1182/blood-2003-08-2724
Jackman RP, Deng X, Bolgiano D, Utter GH, Schechterly C, Lebedeva M, Operskalski E, Luban NL, Alter H, Busch MP, Slichter SJ, Norris PJ (2014) Leukoreduction and ultraviolet treatment reduce both the magnitude and the duration of the HLA antibody response. Transfusion 54(3):672–680. https://doi.org/10.1111/trf.12317
Heddle NM (1999) Pathophysiology of febrile nonhemolytic transfusion reactions. Curr Opin Hematol 6(6):420–426. https://doi.org/10.1097/00062752-199911000-00012
Sahler J, Spinelli S, Phipps R, Blumberg N (2012) CD40 ligand (CD154) involvement in platelet transfusion reactions. Transfusion clinique et biologique 19(3):98–103. https://doi.org/10.1016/j.tracli.2012.02.003
Wang RR, Triulzi DJ, Qu L (2012) Effects of prestorage vs poststorage leukoreduction on the rate of febrile nonhemolytic transfusion reactions to platelets. Am J Clin Pathol 138(2):255–259. https://doi.org/10.1309/AJCP5H7EKZTGGBKZ
Nash T, Hoffmann S, Butch S, Davenport R, Cooling L (2012) Safety of leukoreduced, cytomegalovirus (CMV)-untested components in CMV-negative allogeneic human progenitor cell transplant recipients. Transfusion 52(10):2270–2272. https://doi.org/10.1111/j.1537-2995.2012.03739.x
Ljungman P (2004) Risk of cytomegalovirus transmission by blood products to immunocompromised patients and means for reduction. Br J Haematol 125(2):107–116. https://doi.org/10.1111/j.1365-2141.2004.04845.x
Blumberg N, Heal JM, Gettings KF, Phipps RP, Masel D, Refaai MA, Kirkley SA, Fialkow LB (2010) An association between decreased cardiopulmonary complications (transfusion-related acute lung injury and transfusion-associated circulatory overload) and implementation of universal leukoreduction of blood transfusions. Transfusion 50(12):2738–2744. https://doi.org/10.1111/j.1537-2995.2010.02748.x
Bueno JL, Garcia F, Castro E, Barea L, Gonzalez R (2005) A randomized crossover trial comparing three plateletpheresis machines. Transfusion 45(8):1373–1381. https://doi.org/10.1111/j.1537-2995.2005.00215.x
Baruah S, Bajpai M (2020) Comparative assessment of single-donor plateletpheresis by Haemonetics® MCS® plus and Trima Accel®. Asian J Transfus Sci 14(1):23–27. https://doi.org/10.4103/ajts.AJTS_138_17
Sintnicolaas K, van Putten WL (1993) Comparison of four filters for leukocyte depletion of single donor plateletapheresis products. Transfus Sci 14(2):211–215. https://doi.org/10.1016/0955-3886(93)90033-Q
Heddle NM, Blajchman MA, Meyer RM, Lipton JH, Walker IR, Sher GD, Constantini LA, Patterson B, Roberts RS, Thorpe KE, Levine MN (2002) A randomized controlled trial comparing the frequency of acute reactions to plasma-removed platelets and prestorage WBC-reduced platelets. Transfusion 42(5):556–566. https://doi.org/10.1046/j.1537-2995.2002.00094.x
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17(19):2265–2281. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19%3c2265::aid-sim918%3e3.0.co;2-b
Dzik WH, Anderson JK, O’Neill EM, Assmann SF, Kalish LA, Stowell CP (2002) A prospective, randomized clinical trial of universal WBC reduction. Transfusion 42(9):1114–1122. https://doi.org/10.1046/j.1537-2995.2002.00182.x
Mishima Y, Tsuno NH, Matsuhashi M, Yoshizato T, Sato T, Ikeda T, Watanabe-Okochi N, Nagura Y, Sone S, Kurokawa M, Okazaki H (2015) Effects of universal vs bedside leukoreductions on the alloimmunization to platelets and the platelet transfusion refractoriness. Transfus Apher Sci 52(1):112–121. https://doi.org/10.1016/j.transci.2014.11.001
Yazer MH, Podlosky L, Clarke G, Nahirniak SM (2004) The effect of prestorage WBC reduction on the rates of febrile nonhemolytic transfusion reactions to platelet concentrates and RBC. Transfusion 44(1):10–15. https://doi.org/10.1046/j.0041-1132.2003.00518.x
Picker SM, Steisel A, Gathof BS (2009) Evaluation of white blood cell- and platelet-derived cytokine accumulation in MIRASOL-PRT-treated platelets. Transfus Med Hemother 36(2):114–120. https://doi.org/10.1159/000203359
Kluter H, Bubel S, Kirchner H, Wilhelm D (1999) Febrile and allergic transfusion reactions after the transfusion of white cell-poor platelet preparations. Transfusion 39(11–12):1179–1184. https://doi.org/10.1046/j.1537-2995.1999.39111179.x
Sharma RR, Marwaha N (2010) Leukoreduced blood components: advantages and strategies for its implementation in developing countries. Asian J Transfus Sci 4(1):3–8. https://doi.org/10.4103/0973-6247.59384
Funding
Open Access funding enabled and organized by National Yang Ming Chiao Tung University.
Author information
Authors and Affiliations
Contributions
S.H. Chien and C.Y. Liu organized this study, S.H. Chien and H.Y. Huang performed biostatistical analysis, W.C. Chen and S.H. Chien reviewed transfusion reactions, Y.C. Tsai and S.H. Liu recorded and collected transfusion orders, L.H. Lee and H.M. Liu applied an institutional broad review, W.C. Chen, Y.C. Liu, and T.A. Lin collected data and clinical information, Y.J. Chen checked data quality, S.H. Chien and C.Y. Liu prepared and approved manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Declarations
This study was approved by the Institutional Ethical Committee of Taipei Veterans General Hospital, and the study protocol was in agreement with the Helsinki Declaration of 1975, revised in 2008.
Disclaimer
The funding source had no role in this study design or publication.
Competing of interest.
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chien, SH., Huang, HY., Chen, YJ. et al. Comparing transfusion reactions between pre-storage and post-storage leukoreduced apheresis platelets: an analysis using propensity score matching. Ann Hematol 103, 1389–1396 (2024). https://doi.org/10.1007/s00277-024-05652-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05652-9