Abstract
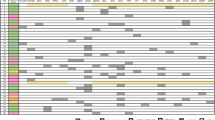
Venetoclax (VEN), a BCL-2 inhibitor, has transformed treatment strategies for elderly and unfit acute myeloid leukemia (AML) patients by significantly improving response rates and survival. However, the predictive factors for VEN efficacy differ from traditional chemotherapy. The clinical relevance of the FAB (French-American-British) monocytic subtype, including M4 and M5, has been debated as a marker for VEN resistance. This real-world study examined 162 newly diagnosed (ND) and 85 relapsed/refractory (R/R) AML patients who received VEN-based therapy at West China Hospital, Sichuan University, from January 2019 to January 2023. We retrospectively collected clinical and treatment data from electronic medical records. The median age of the cohort was 55.5 years (range: 16.5–83.5). The composite complete remission (cCR) rate in the entire cohort was 60.7%. Specifically, among newly diagnosed (ND) patients, FAB monocytic subtypes exhibited lower cCR compared to non-monocytic subtypes (55.1% vs. 76.3%, P = 0.007). Additionally, there were no significant differences observed between M4 and M5 subtypes, both in the ND group (61.7% vs. 40.9%, p = 0.17) and the R/R group (38.2% vs. 40%, p > 0.9). Furthermore, the median follow-up was 238 (range: 7–1120) days. ND patients with monocytic subtypes had shorter overall survival compared to non-monocytic subtypes (295 days vs. not reached, p = 0.0017). Conversely, R/R patients showed no such difference (204 vs. 266 days, p = 0.72). In summary, our study suggests that the FAB monocytic subtype can predict VEN resistance and shorter survival in ND AML patients. Moreover, there is no significant distinction between M4 and M5 subtypes.






Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Nagel G, Weber D, Fromm E et al (2017) Epidemiological, genetic, and clinical characterization by age of newly diagnosed acute myeloid leukemia based on an academic population-based registry study (AMLSG BiO). Ann Hematol 96:1993–2003. https://doi.org/10.1007/s00277-017-3150-3
Wei AH, Montesinos P, Ivanov V et al (2020) Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood 135:2137–2145. https://doi.org/10.1182/blood.2020004856
Kantarjian HM, Thomas XG, Dmoszynska A et al (2012) Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol 30:2670–2677. https://doi.org/10.1200/JCO.2011.38.9429
DiNardo CD, Pratz K, Pullarkat V et al (2019) Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 133:7–17. https://doi.org/10.1182/blood-2018-08-868752
DiNardo CD, Pratz KW, Letai A et al (2018) Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Lancet Oncol 19:216–228. https://doi.org/10.1016/S1470-2045(18)30010-X
Cherry EM, Abbott D, Amaya M et al (2021) Venetoclax and azacitidine compared with induction chemotherapy for newly diagnosed patients with acute myeloid leukemia. Blood Adv 5:5565–5573. https://doi.org/10.1182/bloodadvances.2021005538
DiNardo CD, Jonas BA, Pullarkat V et al (2020) Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med 383:617–629. https://doi.org/10.1056/NEJMoa2012971
DiNardo CD, Maiti A, Rausch CR et al (2020) 10-day decitabine with venetoclax for newly diagnosed intensive chemotherapy ineligible, and relapsed or refractory acute myeloid leukaemia: a single-centre, phase 2 trial. Lancet Haematol 7:e724–e736. https://doi.org/10.1016/S2352-3026(20)30210-6
Döhner H, Wei AH, Appelbaum FR et al (2022) Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 140:1345–1377. https://doi.org/10.1182/blood.2022016867
Bennett JM, Catovsky D, Daniel MT et al (1976) Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol 33:451–458. https://doi.org/10.1111/j.1365-2141.1976.tb03563.x
Pei S, Pollyea DA, Gustafson A et al (2020) Monocytic subclones confer resistance to venetoclax-based therapy in patients with acute myeloid leukemia. Cancer Discov 10:536–551. https://doi.org/10.1158/2159-8290.CD-19-0710
White BS, Khan SA, Mason MJ et al (2021) Bayesian multi-source regression and monocyte-associated gene expression predict BCL-2 inhibitor resistance in acute myeloid leukemia. NPJ Precis Oncol 5:71. https://doi.org/10.1038/s41698-021-00209-9
Gorczyca W (2004) Flow cytometry immunophenotypic characteristics of monocytic population in acute monocytic leukemia (AML-M5), acute myelomonocytic leukemia (AML-M4), and chronic myelomonocytic leukemia (CMML). Methods Cell Biol 75:665–677. https://doi.org/10.1016/s0091-679x(04)75028-1
Kuusanmäki H, Leppä A-M, Pölönen P et al (2020) Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia. Haematologica 105:708–720. https://doi.org/10.3324/haematol.2018.214882
Zong L, Yin M, Kong J et al (2023) Development of a scoring system for predicting primary resistance to venetoclax plus hypomethylating agents (HMAs) in acute myeloid leukemia patients. Mol Carcinog 62:1572–1584. https://doi.org/10.1002/mc.23600
Snijder B, Vladimer GI, Krall N et al (2017) Image-based ex-vivo drug screening for patients with aggressive haematological malignancies: interim results from a single-arm, open-label, pilot study. Lancet Haematol 4:e595–e606. https://doi.org/10.1016/S2352-3026(17)30208-9
Kuusanmäki H, Kytölä S, Vänttinen I et al (2023) Ex vivo venetoclax sensitivity testing predicts treatment response in acute myeloid leukemia. Haematologica 108:1768–1781. https://doi.org/10.3324/haematol.2022.281692
Waclawiczek A, Leppä A-M, Renders S et al (2023) Combinatorial BCL2 family expression in acute myeloid leukemia stem cells predicts clinical response to azacitidine/venetoclax. Cancer Discov 13:1408–1427. https://doi.org/10.1158/2159-8290.CD-22-0939
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127:2391–2405. https://doi.org/10.1182/blood-2016-03-643544
EQUATOR Network | Enhancing the QUAlity and Transparency Of Health Research. https://www.equator-network.org/. Accessed 28 Sep 2023
Cheson BD, Bennett JM, Kopecky KJ et al (2003) Revised recommendations of the International Working Group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol 21:4642–4649. https://doi.org/10.1200/JCO.2003.04.036
Xu J, Jorgensen JL, Wang SA (2017) How do we use multicolor flow cytometry to detect minimal residual disease in acute myeloid leukemia? Clin Lab Med 37:787–802. https://doi.org/10.1016/j.cll.2017.07.004
(2017) Common Terminology Criteria for Adverse Events (CTCAE). https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf
Jiang H, Wei X, Chang C et al (2022) Phase I study of TQB3455, a selective inhibitor of IDH2 with favorable safety and more potent efficacy to IDH2-R172K mutation, for acute myeloid leukemia and myelodysplastic syndrome. Blood 140:9082–9083. https://doi.org/10.1182/blood-2022-164984
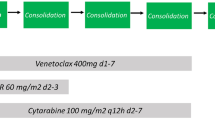
DiNardo CD, Lachowiez CA, Takahashi K et al (2021) Venetoclax combined with FLAG-IDA induction and consolidation in newly diagnosed and relapsed or refractory acute myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol 39:2768–2778. https://doi.org/10.1200/JCO.20.03736
Lachowiez CA, Reville PK, Kantarjian H et al (2022) Venetoclax combined with induction chemotherapy in patients with newly diagnosed acute myeloid leukaemia: a post-hoc, propensity score-matched, cohort study. Lancet Haematol 9:e350–e360. https://doi.org/10.1016/S2352-3026(22)00076-X
Brandwein JM, Saini L, Geddes MN et al (2020) Outcomes of patients with relapsed or refractory acute myeloid leukemia: a population-based real-world study. Am J Blood Res 10:124–133
DiNardo CD, Tiong IS, Quaglieri A et al (2020) Molecular patterns of response and treatment failure after frontline venetoclax combinations in older patients with AML. Blood 135:791–803. https://doi.org/10.1182/blood.2019003988
Pollyea DA, Pratz K, Letai A et al (2021) Venetoclax with azacitidine or decitabine in patients with newly diagnosed acute myeloid leukemia: Long term follow-up from a phase 1b study. Am J Hematol 96:208–217. https://doi.org/10.1002/ajh.26039
Aldoss I, Yang D, Aribi A et al (2018) Efficacy of the combination of venetoclax and hypomethylating agents in relapsed/refractory acute myeloid leukemia. Haematologica 103:e404–e407. https://doi.org/10.3324/haematol.2018.188094
Pei S, Shelton IT, Gillen AE et al (2023) A novel type of monocytic leukemia stem cell revealed by the clinical use of venetoclax-based therapy. Cancer Discov 13:2032–2049. https://doi.org/10.1158/2159-8290.CD-22-1297
Lachowiez CA, Loghavi S, Zeng Z et al (2023) A phase Ib/II study of ivosidenib with Venetoclax ± Azacitidine in IDH1-mutated myeloid malignancies. Blood Cancer Discov 4:276–293. https://doi.org/10.1158/2643-3230.BCD-22-0205
Pollyea DA, Pratz KW, Wei AH et al (2022) Outcomes in patients with poor-risk cytogenetics with or without TP53 mutations treated with venetoclax and azacitidine. Clin Cancer Res Off J Am Assoc Cancer Res 28:5272–5279. https://doi.org/10.1158/1078-0432.CCR-22-1183
Lachowiez CA, Loghavi S, Furudate K et al (2021) Impact of splicing mutations in acute myeloid leukemia treated with hypomethylating agents combined with venetoclax. Blood Adv 5:2173–2183. https://doi.org/10.1182/bloodadvances.2020004173
Winters AC, Gutman JA, Purev E et al (2019) Real-world experience of venetoclax with azacitidine for untreated patients with acute myeloid leukemia. Blood Adv 3:2911–2919. https://doi.org/10.1182/bloodadvances.2019000243
Feld J, Tremblay D, Dougherty M et al (2021) Safety and efficacy: clinical experience of venetoclax in combination with hypomethylating agents in both newly diagnosed and relapsed/refractory advanced myeloid malignancies. HemaSphere 5:e549. https://doi.org/10.1097/HS9.0000000000000549
Venugopal S, Maiti A, DiNardo CD et al (2021) Decitabine and venetoclax for IDH1/2-mutated acute myeloid leukemia. Am J Hematol 96:E154–E157. https://doi.org/10.1002/ajh.26122
Zhang K, Zhang X, Xu Y et al (2023) Efficacy of venetoclax combined with hypomethylating agents in young, and unfit patients with newly diagnosed core binding factor acute myeloid leukemia. Blood Cancer J 13:155. https://doi.org/10.1038/s41408-023-00928-1
Taube F, Georgi JA, Kramer M et al (2022) CEBPA mutations in 4708 patients with acute myeloid leukemia: differential impact of bZIP and TAD mutations on outcome. Blood 139:87–103. https://doi.org/10.1182/blood.2020009680
Zhang H, Nakauchi Y, Köhnke T et al (2020) Integrated analysis of patient samples identifies biomarkers for venetoclax efficacy and combination strategies in acute myeloid leukemia. Nat Cancer 1:826–839. https://doi.org/10.1038/s43018-020-0103-x
Acknowledgements
We thank all study participants for their support.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This work supported by the National Natural Science Foundation of China (82370171) and Sichuan Provincial Academic and Technical Support Funding Project, Grant/Award Number: 2022YFS0191, 00402053A29RY.
Author information
Authors and Affiliations
Contributions
Study conception and design: L.Z., J.J.Y., M.R.C., and Y.W.; development of methodology: L.Z., J.J.Y., and M.R.C.; acquisition of data: L.Z., and J.J.Y.; statistical analysis: L.Z., J.J.Y., X.R.X., and Y.W.; writing:L.Z.; reviewing and editing: J.J.Y., L.Z., X.R.X., and Y.W.; directing and coordinating diagnostic and therapeutic interventions for patients: H.B.M., T.N., Y.P.G., X.C.C., and J.Z.L.. all authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
The study was approved by the West China Hospital Institutional Review Board and in accordance with the Helsinki declaration.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, L., Yang, J., Chen, M. et al. Myelomonocytic and monocytic acute myeloid leukemia demonstrate comparable poor outcomes with venetoclax-based treatment: a monocentric real-world study. Ann Hematol 103, 1197–1209 (2024). https://doi.org/10.1007/s00277-024-05646-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05646-7